Progress
Written by: Keith and Ginny Birrell

Highlight of the week: A gorgeous stay at KuKaya resets us.
Lowlight of the week: We have gone off the Kapani leopard big time. We lose a close canine friend.
Maximum temperature: 41 Celsius
Rainfall: Only sweat, blood and tears.
One step forward. Two steps to the side. A knight’s move. There may be a plan. But that plan is not obvious to the casual observer. This week I’m musing about big data. Big data in Little Luangwa.
It’s 2015. Middlesbrough, England. We have been talking about going paper-free for years. Our trust is way behind the times. And yet, we don’t seem to be able to get our act together. Could it be a money thing? Do we lack computer know-how? Is the Boss not wearing the right trousers? Keith’s practice went paper free in the 1990s. I remember his angst at losing his little Lloyd George notes. He grumbled that his consultations would slow. But Lloyd George was cancelled overnight. Herrington Medical Centre progressed. The hand-written word died quietly. Fifteen years later, we are cajoled by the Trust to be the first department to bite the bullet at James Cook. Young and dynamic. Ready to evolve. Evolve is our new system. Naïvely we agree.
The bullet is bitter and takes some digestion. It takes about a year for Evolve to become fully embedded. Plenty of ward rounds crash and reboot. We falter as the computer says No! The tightrope seems impossible to tread. Paper in one hand. A computer in the other. Carrying both is perilous. Continuity ever important. Effective medical records the key to effective care. For 6 months we use both. Painstakingly we tolerate the duplication. Inching along to an elusive and ever distant goal. But we get there.
It’s 2020. The pandemic hits. We feel smart and smug. We are still the only paper free department at James Cook. We can work from home. Do clinics from home. Check on patients from home. Because all of our records are electronic. Paediatrics has evolved to like Evolve.
Fast forward to 2025. The rest of James Cook hospital is still dithering over its IT options. Our young and dynamic department can crow. Rest on our laurels. Mr Darwin could have written about this many years ago. Only the fittest will survive. Evolve and progress. Change and time marches on. Make the wrong choices and regress. The wrong beak on the wrong finch. Betamax videos. The Sinclair C5. The past is littered with also-rans. Likewise, the writing seems to be on the wall for paper. But what is good for Peter is not always good for Paul. Can Zambia embrace computerised medical records?
The sky is blue in South Luangwa 180 days per year. So a bit of blue sky thinking here would not be out of place. Our blue sky future in Kakumbi might include a virtual clinic network, permitting constant access to online records. Furthermore, the consistent coding of diagnoses and medications could permit Mambwe district to send us all the stock that we need, when we need it. For those of you who are currently indulging in blue sky thinking don’t let this particular Debbie downer burst your bubble for now…….
Even blue skies can turn cloudy - and so, we take the rough with the smooth. We are married to this Valley. In 2021, we made a vow: to return as Valley doctors for ten years, one annual stint at a time. Like any marriage, this commitment calls us to face sickness with health, year after year. For a decade, we stand by that promise.
There is massive contrast here between richer and poorer. We are funded to be here by the rich. Allowing us to champion the poor. Our ebony groves and mopane woodlands are not the same refuge as Sherwood forest though. There is no robbing, nor Robin here. But our time and expertise is gifted to the poor nonetheless. The rich give to the poor.
For better, for worse. While we’d like to believe that 'better' is always within reach, our experience as old African hands has taught us to expect the 'worse' too. The recurring frustration of empty drug shelves has nudged us to think differently - and so, we’ve leaned heavily into lifestyle medicine. Gently, we’ve placed many of our eggs in the fitness basket. Traditionally, Zambian culture has celebrated the status symbol of large bellies and buttocks. Yet, here in the Valley, we’ve made real progress in promoting the value of slimmer waistlines. Our converts have shaped their bums and tums - without skinny jabs. Even when the shelves are full: lifestyle is better, not worse, than medicine.
In 2025, the enduring vow takes on renewed importance: forsaking all others. In an age of overindulgent choice and instant access, that promise can seem outdated - almost trite. But in a ‘Trumpian’ Africa, where USAID support teeters on the edge, every tool to prevent Kachilombo cha AIDS must be embraced. We understand that men here will be men, and women will be women - so we offer some choice: Condoms. Circumcision. Or monogamy. But the greatest of these is love. Or... should that be faith?
Forgive me the digression - I do want to talk about big data and progress. But progress means little without first understanding the direction of travel. For now, I’m still making knight’s moves, opening the game with a few cautious gambits. Our VSO training in 1994 taught us patience: wait, watch, learn. After four tours of duty we now match the record here, totalling 15 months of round-the-clock service. That time has earned us the right to speak about how things really are - in our clinic, and in our community.
Over our four tours of duty, we’ve witnessed many changes here in Zambia. Some have undoubtedly been for the better - but others, not so much. Drug supplies remain inconsistent: occasional feasts, but more often, famine. The clinic has been especially quiet these past two weeks, likely due to a current drug shortages. We are, once again, in the midst of a famine. It’s fascinating to observe how health-seeking behaviour shifts in response. Patients know we have few medicines to offer, so many bypass us entirely and head straight to the pharmacy - where a cornucopia of pills awaits. There, with just a hint of their symptoms, patients and pharmacists collaborate to pull a mix of brightly coloured packets off the shelves. But medicines cost money, so they often leave with just two or three of everything: a couple of antibiotic tablets, some painkillers, a few vitamins. When they start to feel better - usually because their self-limiting illness has run its course - they stop taking the medication altogether. Not because the tablets worked, but in spite of them. And so, the cycle continues: antibiotic misuse rises, and antibiotic resistance grows, false health beliefs are reinforced. The pharmacists prosper - and so does Big Pharma.
Many believe that data holds the key to solving this riddle. Data is power. Data is knowledge. Data is money. We need to understand what illnesses people are experiencing, what medications they require, and how many patients the clinic actually serves. When you control the data, you can control the drugs. Monitor usage. Improve supply chains. Deliver the right medicines. In the right amounts. At the right time.
It's 2021, the clinic runs entirely on paper records. Each patient has a book, stored on-site. Retrieved and used at every visit. A diagnosis is required and recorded in a large ledger. Along with any prescribed medication - a system that creates a basic record, of sorts. But accuracy is inconsistent. Diagnoses are often imprecise, and prescribing can feel arbitrary. Books go missing. Previous visits are rarely reviewed. Continuity of care is the exception, not the norm. A significant challenge for managing long-term conditions.
Fast forward two years - it’s 2023. To our astonishment, a computer system has been installed. Laptops now sit in every room. The paper is gone. A nationwide government IT health programme has arrived. Zambia, it seems, is ahead of the curve.
Meanwhile, in the UK, the government has spent millions attempting to create a similar nationwide health IT system - one that allows records to be accessed seamlessly across GP practices, community centres, and hospitals. So far, it remains little more than a pipe dream, failing spectacularly despite continued investment. Instead, most UK hospitals have rolled out their own electronic health record systems, with mixed results. Many are clunky. Unpopular with clinicians. Riddled with glitches. Time-consuming to use. Worse still, they don’t interface with primary care - so the whole idea of a connected system remains elusive. With that in mind, we didn’t hold high hopes for Zambia’s new system.
And rightly so. The Zambian system faces immediate challenges: unreliable networks, slow internet, and limited computer skills among staff - most typing with a single finger. It doesn’t seem to enhance consultations in any meaningful way. We are issued logins and, somewhat reluctantly, try to engage with the system. While plenty of data fields exist, most go unused. A few words might be entered under 'presenting complaint', but there is rarely any documentation of history or examination. A basic diagnosis is recorded, followed - when the system allows - by a prescription. When the system goes down, as it often does, we simply revert to books and paper.
Zambia, 2024. And nothing has changed. Poor data in, poor data out. It’s painfully slow, waiting for the system to load - when it works at all. Keith and I inevitably fall back on pen and paper. This is the year of load shedding - or power cuts, as you and I would call them. The clinic’s solar panels rarely work, and no power means no internet, no computers, and no data collection. No big data.
We return in 2025, hopeful for progress. And sadly
Sitting around
Written by: Keith and Ginny Birrell

Highlight of the week: We stand in for Ellie and Crispin to hand out football kits to children. Their joy brings us to tears.
Lowlight of the week: Hot nights and a dripping air conditioner lead to sleep deprivation
Maximum temperature: 41 degrees Celsius
Rainfall: Cloudy skies. A muggy feeling. But alas no rain
Mr Attenborough makes it look easy. His dulcet tones play softly as the backing track to any safari feast for the eyes. But those feasts are in reality surrounded by famine. Hours or days of famine for each feast. And yet the offset is worth it. David can never quite compete with the real time experience. Patience pays dividends. And some.
Our lives now have rhythm. Routine. Balance. In previous years, we have driven into the park ourselves. Twice a week. In search of animals. And nature. Always on the lookout for predators. But happy with anything that moves. As long as it’s not a big grey creature with a trunk bearing down on us. We have always jumped at the slightest opportunity to jump on a proper game drive. To make the most of the unrivalled expertise of South Luangwa guides. To sit in an open game viewing vehicle. To be able to appreciate the sounds and smells of the bush. Heaven for us. Last year, we struggled to get professional drives. Somehow the Valley docs didn’t seem to get much quid pro quo. Belts tightening.
This year, our friendships with guides has paid dividends. With private drives most Sundays. Often shared with Ellie and Crispin, who are having an extended break out here. Now there is no fear of us ruining the trip with an emergency call. Our agenda is top of the bill. Or at least a close second behind the possibility of a sudden serious medical crisis in the Valley.
I will spare you the detail of how a drive in our park unfolds. I’ve waxed about this before. Occasionally it gets lyrical. Rituals My blog tends to focus on the action. Skipping the hum drum. Not mentioning the hours spent driving down dusty roads. Eating other cars’ dust. Being eaten by tsetse flies. Chainsaw mouth parts penetrating denim, elephant hide or armour plating. The expectation of working to a particular wish list counterproductive. We create luck through patience. Luck comes from hard work and application. The bottom line is that we focus on process not outcome. Each minute is mindful. We appreciate the peace, the noises. The smells, the stenches. The beauty, the horror. We marvel at the light, the wilderness. But an Attenborough grade sighting always rocks. And this is catalysed by all the waiting, watching, appreciating. Letting the wild world play out.
We switch things up this weekend. Rather than an early Sunday morning drive, we plump for Sunday evening. Setting off at 16:00. As the air cools. The sun low in the sky. Sleepy animals start to stir. Predators realise that they have to re-earn their repute. A gaping yawn. Bare teeth. Tongue smacks lips. Wide eyes view the plain. Check out the evening menu. Carnivore style.
The dream is to find apex predators mid-selection. Viewing the smorgasbord. Picking out a buffalo, an impala or a puku. Executing a stealthy approach. Clinically dispatching their choice. Carving up the freshest cuts. Bolting their dinner. Wanting the lion’s share. Regardless of their ilk. No desire to savour or share. Certainly unwilling to welcome competition.
Now is the golden hour. When the light is at its best. Lighting up the vegetarians as they too bolt their few last mouthfuls. Lighting up Valley docs as they toast the dying sun. Together with their expert guides. The contrasts make great copy for the blog. And now the night life is truly alive. Squinting baboons and puku send off alarm calls. Warning friends and colleagues that mischief is afoot. Summoning Keith and Ginny to chase the bad guys away.
Daniel, our guide, has a plan. Let’s look around Riverside drive. Head to Wamilombe. Aim to have sundowners by the river. We don’t want to tick boxes. We are happy for Daniel to set the agenda. An agenda that will be set by patience and whatever the bush wishes to offer.
We stop by the Mfuwe lagoon to check out the birds. Crocs. Grazers chancing their necks for a quick drink. Another vehicle approaches. Two guides exchange sightings in code. The bush telegraph in action. We know a few words in the local dialect of Kunda. We listen out for: Kaingo – Leopard; Nkalamu - Lion; Mbwa - Wild dogs. Key elements tell of a deeper story. Our guides mix up Kunda, Nyanja and English. Preventing even Mr Turing from gaining full access. Yet it whets out appetites and keeps your average safari goer out of the loop. It makes sense for the chatter to be unintelligible to the tourists. The guides don’t want tourists to have false hopes. And perhaps they also want the kudos of an apparently fresh find. Teamwork disguised. The bush talks to those who know how to listen.
I hear nkalamu. An earlier sighting. In Wafwa. The Dead river. An oxbow. In the opposite direction to our trajectory. As our guides sit talking, 3 vehicles go past. Heading to Wafwa. Daniel turns to us. To share the news. Do we want to go to see the lions? Keith and I glance at each other. An imperceptible shake of the head. We are far too discerning for that. Picky. Hard to please. Lions are incredible. Beautiful predators. But its 16:15. The sun is still high. We know they will be sleeping. Surrounded by safari vehicles. Jostling for position. So guests can get the best photos. Ticking off their lists. We like exclusivity. And if we are going to share, we like action. We tell Daniel to stick with the original plan. He smiles and looks relieved.
We wind our way towards Riverside drive. But branch off unexpectedly. We divert toward the now dry Mbangula lagoon. We pass a couple of cars coming in the opposite direction. Daniel knows something that we don’t know. As we round the corner, he tells us. There is a leopard over there. Lying in the grass. We fish out our binoculars. And gaze into the grasses. Fifty metres away we can just make out the shape of a sleeping leopard. There are already 4 other vehicles here. A big give away. Daniel positions us with the best view. We tell him we are set. Let’s just stay here. To see what happens.
We stay put. Cars come and go. Tourists get to see a distant leopard. Put a tick in the box. And then head off, in search of lions. We do not move. Our leopard stirs. Sits up. Looks around. Yawns. And goes back to sleep. We try to figure out which leopard it is. It’s not Lucy. It seems too small? Or perhaps it’s just far away? It has to be one of Lucy’s cubs.
The sun is going down. Keith suggests we have our sundowners in the car. Right here. Sundowner time catalyses cats into action. And our index feline needs a nudge. Keith reaches into the cool bag. Suddenly, there is action. We hear monkeys barking. Squirrels chirping. Have they just spotted the invisible spotted cat in the long grass? Could there another predator around? Perhaps Lucy is bringing an early supper. Or maybes the twin brother is on the prowl? We train our binoculars on the leopard. He gets up. Stretches. And moves 5 metres to his right. Only to settle down again. We look around hopefully. But the bush falls silent again. Monkeys and squirrels have short memories. They were squawking at our leopard. And have now forgotten that he is here.
To our left we hear the unmistakeable chatter of guinea fowl. My least favourite animal. Keith loves to tease me: He plans to get a flock for our Yorkshire home: Kwetu. During our Zanzibari adventure, all those years ago, we were surrounded by guinea fowl. Owned by one of our neighbours. Every morning without fail, they would wake up with the sun. And start their endless chatter. Outside our bedroom window. An immutable alarm clock. The noise mainlining into my limbic system. My brain automatically on edge. Inviting me to wring their necks.
Guinea fowl necks are made for wringing. Nick, our North Yorkshire neighbour, was unable to quell the urge last year. He kept 3 guinea fowl as pets. But their cock would pace up and down all night. Chattering. Squawking. Fretting. Nick’s sleep deprivation triggered a reflex fugue. The cock guinea fowl did not see the night out. Three became two.
The guinea fowl are noisily making their way towards the trees. To roost for the night. They have chosen a precarious path. Right past our leopard. Hearing their noisy chatter, he lifts his sleepy head. Ears twitching. Nose sniffing. Well camouflaged. Switching from off to on. He stays still. The first of the birds go on by. Reaching safety through good fortune. Oblivious to the predator in the grass. The second group approach. I direct them toward their executioner. With a virtual tractor beam. The birds have no choice. They gravitate towards a bloody end. But suddenly the quality of their chatter changes. From a mindless grating squawk to an insistent screaming noise. They have spotted our spotted cat. But they don’t run away. They go closer even to investigate. We are on edge. Binoculars glued. Could this be my wish come true? A really annoying bird killed by a cat with a penchant for bush chicken? But our leopard isn’t really interested. He is already worldly wise. Aware that wings can take his fast food away fast. He fails to be baited. The fowl remain foul.
Keith hypothesises that the only way to make our leopard move again is to get the drinks out. Barely has he got 2 cans of tonic out, and our leopard stretches and yawns again. One time. Two times. The magic three times. This is a sign that a leopard is really getting going. Our boy is taunting us. It takes another 15 minutes before he stands up and properly stretches. By now we have been waiting in the same spot for 90 minutes. Only one other car is with us. One other set of patient cat lovers. Here for the behaviour and the action. Not just the tick. Of course, the sun is now going down. We have missed the golden hour. The light rapidly fades. My camera barely records the moment. He saunters down the bank to a track. 30 metres away. We follow from across the dry pock-marked lagoon. Somehow, our Landcruiser lurches through the elephant and hippo holes. But courtesy dictates that we allow our fellow vehicle to precede us. Our leopard elusively beyond our gaze.
Soon the young feline tires of the chasing tyres and heads into the bush. And the other vehicle quickly loses interest and races off for a late sundowner drink. But Daniel reads the cub’s mind. We nudge back into the bush ahead of his trajectory. And wait. Our lights search out his eyes. Cat’s eyes betray him. Inquisitively, he follows this new tractor beam and almost jumps into Keith’s lap. Keith resists the instinct to stroke. Stroke prevention seems so sensible here. He has spent so much time in Zambia banging on about. He takes a swig of his own medicine. Stroke prevented!
Up close and personal we realise that our leopard is really quite small. Certainly one of Lucy’s cubs. A year old now. Eye contact makes the experience all the more personal. Our breath suspended. No hint of malice in these inquiring eyes. Our Landcruiser might have a spare seat for me he enquires. Instead, he decides to stroll on by foot. Moving more sitting less, he echoes our stroke programme chant. He leads we follow. Daniel’s vehicle capable and versatile. He gives us 15 minutes of fame. We are blown away. Our closest leopard encounter ever. Exclusive. Personal. Special. Magical.
Saint Daniel is beatified. The most patient of all saints. After the crescendo, our evening apparently complete, we start to wend our way back towards our own Doc car, parked at Mfuwe lodge. Mzungu also patient. Our minds’ eyes replay our magical encounter. Retinally persistent against the black night. The moonless night is otherwise broken only by Jaffet’s searchlight. But our virtual movie is now broken by our guides’ relentless talent at finding leopards. Lucy herself summoned by the Jaffet’s tractor beam.
Lucy crosses the road in front of us. From nowhere. With a flattened left ear. Unmistakable. She is on the hunt. Stalking a waterbuck. Out in the open. We watch her, spellbound. Our white searchlight is quickly swapped to a red light. Not interfering with the hunt. She settles in the grass and watches. With the patience of a leopard. A new superlative. Second only to the patience of a Daniel. We wait for an age. And then conclude that the waterbuck is too far away. And way too big for her. She seems to reach this same conclusion. At the same time. We feel the pull of the park gate curfew and head off. But so does Lucy. All of us see some distant impala. There are no crows flying there, but Lucy stalks. We place ourselves in front of the impala. Right in Lucy’s way.
Lights off. We sit tight. The park curfew badgering us. Other vehicles fail to spot us in stealth mode. They head off. But Daniel knows that we have a trump card. Our Doc status allows us to blag a little. We have a medical situation here of sorts. Someone is due to get hurt. Daniel’s instinct is to stay dark. To keep the encounter exclusive. To avoid breaking the magic spell. The deathly dance of predator versus prey. Ours. Alone.
The impala munch. Nearby elephants casually pull down tree branches. Eating succulent leaves. Our light flicks on Lucy in timelapse fashion. Nearing. Initially imperceptibly. On dramatic paws. Then Lucy runs right at Keith. Like son. Like mother. She launches herself towards our Landcruiser. And then she’s gone. At least from my view. Keith breathes again. Neck intact. Lucy has ducked underneath us. Daniel has her by his feet.
We look over the right side of the vehicle. Under our spare wheel. Lucy’s head pokes out. She is one with our car. Using us. Shameless. She is poised.&
Diagnosis
Written by: Keith and Ginny Birrell

Highlight of the week: Two become three as Joel joins the Kapani set
Lowlight of the week: Elephants claim a 5th victim
Maximum temperature: 38 degrees Celsius
Rainfall: Only in our dreams
It seems important. Putting sick people into categories. Giving them labels.
Clinicians love a diagnosis. People become patients. With that comes the permission to treat. The possibility of cure.
But the sword is double edged. Cutting both ways. Curing in one direction. Carving up when wielded carelessly. A diagnosis often delivers collateral damage.
This week finds me on the trail of a diagnosis. But the trail is fraught with hazards. The goal illusory. Come and explore with me. I’m working at our new District General Hospital. Velos.
I am really enjoying my mornings at Velos. The new district hospital. I guess I’m an acute paediatrician after all. I’ve worked in the Zambian primary care environment for 4 years. Sometimes it is stimulating. But often my mind wanders. I am not as useful as Keith. He is pulled in several directions every day. Eyes. Ears. Psychiatry. Hypertension. Diabetes. He always seems to be seeing and sorting. General practice is his baby. But even babies aren’t really my baby. I am a little too specialised. Sick children are my thing. And in Kakumbi, they are mostly not properly poorly. Lots of flu. Coughs. Skin rashes. But the staff are now pretty happy to deal with most of this. Their antibiotic stewardship is now pretty hot. The staff dole out small rations of paracetamol. Nowadays, everyone is happy with less being more. Patients expect less drugs. Leaving more medicines for those in real need.
But up at Velos it’s all going on. The threshold for admission is high here. Partly because primary care sorts out the chaff from the wheat. But the bottom line is that people only go to hospital if they really need to. Geography controls the paediatric admission rates, even more than our clinicians do. Nobody has a car. So the rate limiting step for hospital admission is the availability of our single ambulance. Secondary care only takes the crème de la crème. This makes a paediatric ward round interesting and eye opening. Rarities are concentrated. Just what my brain needs. A diet of the weird and the wonderful. Throw in the lack of tests and a limited supply of drugs. And my grey cells can really get stuck in.
Tuesday is our 3rd planned visit to Velos. I arrive on the ward to find the ward round prematurely complete. They forget that I’m coming. But I am now African. I adapt and make a plan. Find a role. Find a niche. Plug away. I help with a difficult cannulation. I chat with staff about shared problems. Pet topics. Challenges. Thorny issues. Pain relief and dressing changes amongst them. A screaming child, the blood curdling backdrop to our conversation. As the morning calms down and the screams subside, we firm up plans for next week's later ward round.
It's 11:30. I go on a Keith hunt. Hoping that he has saved me something that might right up my street. My timing is impeccable. He is looking for me. Gin, come and see this child in the emergency room. His face is swollen. Maybe he has nephrotic syndrome?
I head to our mini-casualty. My brain moves into 2nd gear. I find Peter. Twelve years old. Lying quietly on a bed. Surrounded by concern. The team around him. Two clinical officers. Two nurses. A machine is making an annoying beeping noise. Without a thought, I turn to silence the bleep. But my thoughts suddenly intrude. The numbers make me crash through the gears. Peter is properly sick. His oxygen saturation is 78% on oxygen. His pulse rapid at 120. There is a rabbit away. Or should that be a hare? Whatever. I’m set to chase it. Peter looks chilled. Perhaps too chilled. But with it. Alert. His mother by his side. We start at the beginning. With his story.
Peter has been particularly breathless for 1 week. No cold. No cough. He is not eating well and has some vague tummy pain. No fever. No vomiting. No diarrhoea. No constipation. He reportedly started to swell 2 days ago. His face. His abdomen. His ankles. Prior to this, he seemed well. But mum now admits that for a year he has struggled to walk. Getting a bit tired and breathless. He is doing well at school. He’s a 5th grader. Who wants to work in health.
I look more closely at Peter. In medical school I was taught to start with people’s hands. My clubbing aspirations were not confined to the Stage Door in Newcastle. Clubbing. An indication of serious heart, or lung, conditions. Those conditions do not remain nameless. I reel them off, in those confrontational medical school seminars. Not fully connecting with the personal health challenges owned by the owners of these rounded finger nails. But in my career in paediatrics: only one of my hands has been needed to record the children that I have seen with clubbing. But Peter makes me use my other hand. My hand holds his. To wonder at the convexity. To connect with Peter. To offer him support. But my medical memories break the personal connection with Peter. I now have my hands full with his deteriorating health.
Peter has impressive clubbing. His fingers have small drumsticks on their ends. The like I have never seen. These drumstick beads tells me that his illness has been brewing for some time. Months or years for sure. His pulse is weak. Despite 100% oxygen, his oxygen saturation won’t budge from 80%. He is breathing a bit fast. 28 breaths in a minute. But he is not struggling to breath. No noises. His chest is clear. This is not a lung issue. His heart is sick.
Many of you are medical so I will give you few more clues: his heart is working hard. I can feel it through his chest wall. The right side of his heart is oversized. His heart sounds are interesting. He has a loud 3rd heart sound. No murmur. He has a very swollen abdomen. There is fluid in there. His liver feels big. He has ankle swelling. And facial swelling.
The medical team look to me for answers. I have some. But not the key diagnosis. I announce that he has right sided heart failure. Pulmonary hypertension. His lungs are stiff. The pressure in the lung blood vessels is too high. So his heart cannot push blood into them properly. Each time his heart beats, only a small amount of blood goes through his lungs. A lot of blood takes a shortcut. Probably through a big hole in his heart.
Undiagnosed congenital heart disease. His heart has dodgy plumbing. Scrambled before birth. The blueprints weren’t followed. A decent baby check would have spotted this. Most likely his oxygen levels have been fine for years. But a stethoscope placed on his heart even in those early days would have trumpeted the plumbing issue. If a decent plumber had been called, back in the day, the problem might have been fixable. But more on that later.
Back in present day Zambia we now have some options. Our state of the art, shiny new hospital lets me look inside of Peter’s heart. To see how it’s built and to see why Peter’s heart has gone south. A fancy cardiac ultrasound machine looks at his heart muscle, valves and blood flow. An ECG checks out the heart electrics. Shining a light on Peter’s dark cardiac health. I ask the staff to give Peter some diuretics to nudge his heart in the right direction and reluctantly leave the hospital. My carriage awaits and I can’t risk it turning back into a pumpkin. We have staff to move around the community.
Peter appears to be up a brown murky creek. His paddle is floating hopelessly in the opposite direction. There is nobody willing, or able, to jump out and retrieve the paddle. Despair is our overriding emotion. Keith and I share our very short list of bright ideas as we drive away. We resolve to phone a friend as we stop to pick up our tired, overheated, community staff.
The following day, my phone pings to relay the dark truth inside Peter’s heart. Tetralogy of Fallot in Zambia punctuates lives with too many commas. Pauses for air, in a breathless existence. And a final full stop. Written much too soon.
Peter has undiagnosed congenital heart disease. A problem called Tetralogy of Fallot. A picture I am very familiar with in the UK. Normally diagnosed within hours, if not days, after birth. British babies are sent to a regional paediatric cardiothoracic unit. They may need early surgery. Sometimes they are given medicines until they grow big enough for corrective surgery. But even then: a magical heart operation is performed by 4 months of age. They can usually expect to lead normal lives. Into adulthood and beyond. Paddles in hand. Battling through rapids. Clean water churning under the robust boat that holds them.
Peter’s journey will not be a positive adventure through his short life. He has complications arising from a poorly plumbed and uncorrected heart. We can’t reverse the damage already done to his pulmonary blood vessels. We will never be able to make him pink. His heart failure might be managed. But never cured. He has a very reduced life expectancy. His breathing will get worse. Oxygen unable to get to his brain and vital organs. His body will become water logged. His parents will likely search for support. Better care. Funding to travel. A quest for medicines, an operation. Some hope. But this short essay is likely to come to a heart twisting, premature end.
The diagnosis is now in Peter’s notes. Paper and transitory. Or virtual and subject to network failure. We have no real treatment to speak of. Peter’s diagnosis spells the end of hope in our adopted homeland. Zambia overwhelmed with late diagnoses that overwhelm people and their families.
One lone olive branch reaches out offering solace. Precious gives us hope for Peter. I diagnosed Precious’ congenital heart disease at 3 months of age. (https://keithandginnybirre.wixsite.com/intoafrica/post/getting-to-the-heart-of-the-matter) We wrote about her during our first year in South Luangwa. She lives on, somehow, against poor odds. We plan to see her next month. To chart her unusual Lazarus-style survival. I hope get to a decent picture of her heart now. To figure out the plumbing and to make sure that no stone remains unturned for Precious.
Meanwhile Peter’s plot Peters out. He dies in the night. In the referral hospital 3 hours to our South. The Southward trajectory of his heart complete. The pings on his monitors stop. Full stop.
We wonder at the possibilities of a future Zambia. Where future Peters, born as short stories might be rewritten as epic novels. With new born vigour in a capable health service that includes wonderful hospitals like our own Velos. Could it be possible that Zambia will no longer be the wrong country to be born in with a scrambled heart? Will Zambia be a place where making a diagnosis will really make a difference?
A Testing Time
Written by: Keith and Ginny Birrell
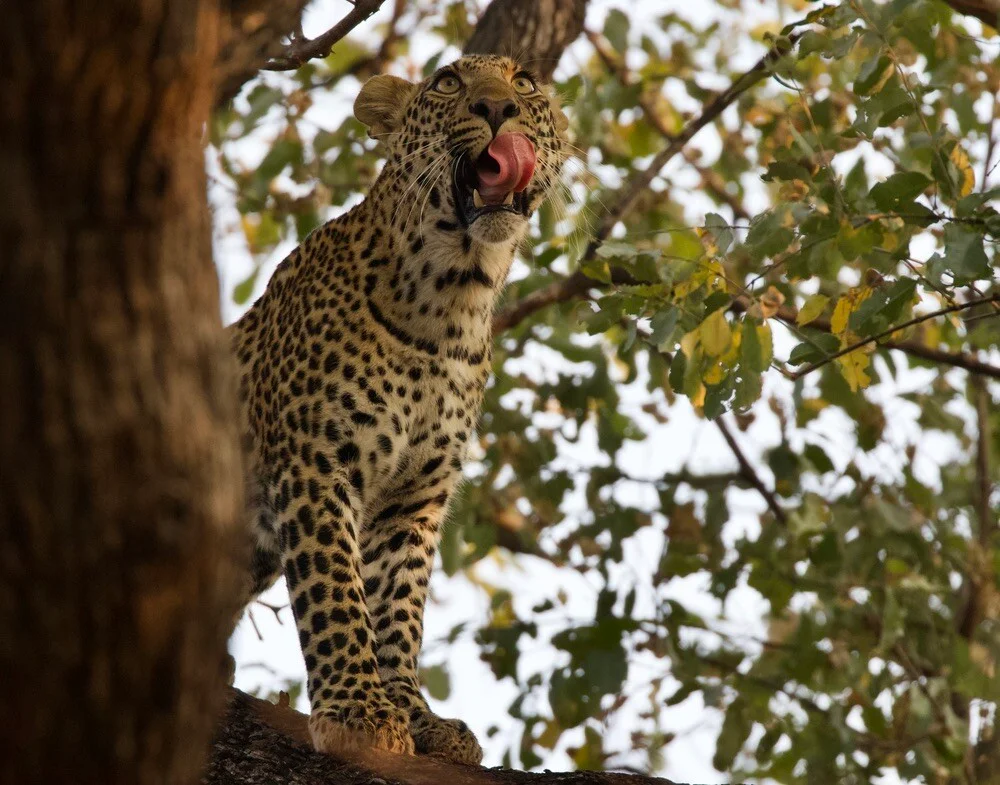
Photo of the week: A new leopard for us - trying to catch monkeys up the tree
Highlight of the week: Close ups with elephants, with no fear
Lowlight of the week: A sick boy with a life sentence
Maximum temperature: 33 Degrees Celsius
Rainfall: Rather dry
The witching hour. Strange medical things that go bump in the night. 02:00 - 04:00. A time best left to the fairies. Not a time for us mere mortals to be troubled. Bizarrely, I have never seen, or been seen, at this time. For the entirety of my career…. So far…. My juniors never needed to call me…..
Evenings in South Luangwa are typically quiet. Gone are our days of raving. Partying ‘til dawn. Going to work on a hangover. Thinking that sleep is for softies. Our middle names are now Responsible. The irrational vigour of youth spent. We crave our due ration of sleep. Downtime part of the mix. Occasional nights out remind us of the heady days of our youth. Yet even those nights fizzle by 21:00. Especially on a school night.
It's 19:30. We have eaten. Taken our antimalarials. Cleared up. Prepared our bags for the morning. It’s wind-down time. I prepare for bed. Crawl under the mosquito net. Read. Chill. The lights should go out at 21:00. But Keith calls out: Don’t get undressed yet. We have work to do.
I’m tired. Bummer. I groan. It has already been a long day. Nowhere near the witching hour. But still, my relaxation plans have been destroyed. Grumpily, I emerge from the bedroom. We steel ourselves for the next bout.
Jack is having some kind of mental health crisis. Can we help? We try to gather more information. We are told that Jack is staying in a camp up the road. He was due to fly out today. But he was too distressed to get on the plane. Could you see Jack? He might need sedation. We do a quick stock check. Oral and intramuscular magic. Cushions for the mind. Medicines that calm and protect. We hop into Mzungu. Our white Hilux. And head toward the camp. Thinking aloud.
Thinking is allowed. Although many clinicians seem to fire from the hip, way too often. A great joy of medicine is the challenge that it offers. No two patients are truly alike. Our shared job as Valley Doc a precious thing. For each conundrum we see things with different eyes. We bring differing views. Approaches. Spin things different ways. Synergistically, not oppositionally. Problems halved or at least shared.
Our journey to see a patient is a crucial phase. Thoughts collected. Approach negotiated. Tasks apportioned. A flexible plan, mapped out. A goal at least. In this way, we arrive with purpose. Our clients see confidence. To inspire confidence. Part of the battle. Anxiety muddies the water. Clarity is needed.
Jack sounds agitated. Clouded thoughts. The product of medical, chemical or psychiatric forces. But we must not jump to false conclusions. Run before we can walk. My task will be to gather information from those around Jack. Keith will aim to engage with Jack.
The phone rings again. There is confusion. Jack is on the move. No longer at camp. His colleagues have taken him to a clinic. But which one? Kakumbi? Or Velos? We stop on the road. Ten minutes triangulating. Velos the new plan. Our drive resumes. Velos is a short schlep. 30 minutes under Mzungu steam.
It’s 21:00. We arrive at Velos hospital in synch’ with Jack. He is sat in the front passenger seat of an open game viewer. Held fast in a caring embrace by a young lady. Settled? We rashly venture. But as we approach, it becomes clear that all is not well.
A flash of anger. Menace. Fearful eyes. Words betray his paranoid state. The car door thrown open. A stare, insistent that Keith should not approach.
Jack’s agitation propels him away from us. Fortunately, the hospital parking lot is a safe space. Well lit. Fenced off and elephant-free. He mutters at nobody in particular. Pacing. His girlfriend heads his way. To shepherd him. At least there is no suggestion of any getaway plan. But Jack’s inner turmoil, and our challenge, won’t be resolved anytime soon.
Whilst our patient mutters and paces, I peel off to focus on my preassigned task. To seek further information from Jack’s colleagues and his partner Lucy. Keith phones a friend. Jack’s best friend. Jack’s brother. Rudi.
No history of fever. No rash. No unusual insect bites. No illness. A four week steady decline in work ability. Change of attitude. Reports of being confrontational. No history of alcohol abuse. No drug use. He hasn’t slept well for the last week. Not at all for the last 24 hours.
Keith speaks to Rudi, one thousand kilometres away. Rudi and Keith share their intel. And then Keith begs a favour: A reference from Rudi that will likely help Keith gain Jack’s trust.
Nothing in the gathered stories suggests an acute medical illness. Nor a toxic response to chemicals. That leaves a psychiatric issue. Acute paranoia. Disturbed thinking, without a physical or so-called organic cause.
The phone is spirited to Jack. Opening an intracontinental dialogue. Initially, Jack’s paranoia puts the kybosh on our preferred way to Jack’s heart and mind. The phone is thrust away. The tarmac impacted by the phone’s resilient case. Strike one. The use of someone else’s phone is eschewed. Not to be trusted. Try harder Doc.
Reaching the end of the opening salvo of our plan: Keith and I reconvene. The plan needs some refinements. Some detail. Some contingencies. Trust is key. A shared plan with patient and docs might involve sleep and calm. Chemically induced calm, for a troubled mind, is best taken by choice. But how do we help Jack to realise that our choice can also be his choice? A photo of Jack’s chosen medicines give Keith an in. Sleepers seem to be an acceptable option. Lucy is tasked to ask Jack if he would like a sleeping tablet. Photo of the week: A new leopard for us - trying to catch monkeys up the tree
Highlight of the week: I find out about the wait-a-bit thornbush. An acacia shrub that keeps predators at bay. Even elephants and buffalo stay clear of its fierce embrace.
Lowlight of the week: The cool of the Zambian summer is over. Our aircon struggles to get with the programme.
Maximum temperature: 38 degrees Celsius
Rainfall: The chance would be a fine thing.
To test, or not to test? That is the question.
The answer might be imposed upon you. It’s 1994. Northern Unguja. Zanzibar. I have 5 tests at my disposal. Malaria. HIV. Haemoglobin. Blood group. Stool parasites. Now what was the question?
Imagine that you are reading my blog from 1994. Malaria is rife. Yet the test is rarely done. HIV is, as yet, rare. And that test is predominantly reserved for donated blood. If a child looks pale, they are pale. A haemoglobin of 2.7 g/dl might surprise you in England. But I am rarely wrong in deciding who needs a transfusion here. Test, or no test. And stool parasites are the rule here, rather than the exception. I treat those that need treatment. Not those that I test.
It’s 1997. We are back in England. Zanzibar is like a hazy dream. A quick backpack trip around the world is now merely a collection of images. Albums that are due to collect dust. I am working in my first registrar post in paediatrics. On a 5 year trajectory to becoming a consultant. Throughout medical school I was indoctrinated with the maxim that 80% of diagnoses could be made from the history. But a panoply of tests challenges my doctrine. Why would all of these tests exist if they weren’t needed? Surely, I should be doing more tests!
I also have a computer. My slave? More likely my master! The screen demands. Expects. Insists. What tests are expected? So many options. A tick in a box. Another test requested. As easy as that. I just need to decide which one. Perhaps just do them all? It’s only one small needle into a vein. A few bottles to fill.
I’m on call with Jonathan. My boss. Not yet a friend. A head appears at the door of the paediatric day unit. Jonathan’s disembodied head seeks permission to depart. Dinner awaits. But his body surrenders an opportunity for an early supper, and leads him right into the day unit. PDU a home from home, for all conscientious paediatricians. Resistance is futile. He offers support. A 3 year old girl is taxing my mind.
She has a mild fever. A red throat. Pink ears. Cervical lymph nodes palpable. Nil else. I think it is a virus infection. But I am toying with doing some blood tests. Because I can. I tell Jonathan I am going to do a full blood count. Why? He asks. I reply confidently: Because if the white count is high, I might give her antibiotics. He looks at me thoughtfully. Do you need a blood test to decide that? What would you have done in Africa? Now that gets me thinking. Just because I can do a test, should I? I go back and look at the child. She is full of snot. Virus is written all over her. What further proof do I need? My clinical skills are good. They have had to be for the last 2 years. Why should a random number influence me? Why do we do tests?
This single conversation guides my route through paediatrics. Steers me. Not off on a tangent mind. But changes my trajectory. Tests have a place. In endocrinology, tests are the mainstay of monitoring and managing endocrine problems. Necessary. Useful. And also in acute situations, they help. Guide. Support. But the key to managing problems is a good history. A thorough examination. Sometimes time. But tests are not a kneejerk response. Any test needs to add value. Some will send you down a convoluted rabbit hole. Harming not helping. Costing and not contributing.
Reflex testing is now part of our NHS culture. Nobody wants to miss that needle in the proverbial haystack. Guidelines have become tramlines. Defensive practice stifles the possibility of clinicians using their clinical acumen. The blunderbuss approach has become standard. And we are all paying for it. No rabbit warren is left unexplored. And the golden goose stays quiet. Why honk when your nest is being feathered by endless, profitable tests?
First, do no harm, Hippocrates advised. Today, he is turning in his grave. His timeless aphorism lies in ruins, replaced by a new mantra: Leave no stone unturned. But in our frantic stone-turning, we’re generating more heat than light - much effort, little clarity, and often, unintended harm. I suggest that we stop turning stones and let Hippocrates lie in peace.
Zambian practice has its virtues. Tests are sometimes present. But geography and supply chain issues ration their use. So time remains my favourite test. Natural history and cold hard clinical symptoms and signs guide us to our holy grail. But progress, of a sort, is marching on. Even in deepest, darkest Africa.
We have our wonderful new hospital, up our single tarmac road. Velos currently houses a number of people with injuries. Including a couple of local men, beaten up by a particularly grumpy elephant. Velos has a beautiful purpose-built lab. Radiology facilities, the envy of any DGH in England. Skilled laboratory technicians. But reagents are like hens teeth in this part of Africa. And for your information our hens have beaks just like yours. So I find myself back in the Africa of yore. Familiar territory. Rejoicing that my 5 tests at least do no harm.
It's Friday. Our Kakumbi clinic is quiet. Keith and I are looking for work. Quite unusual in these parts. I hear a rumour of a sick baby. I gravitate towards the cries. I find Joy. One of our staff members. She is cuddling her son, Martin. He is 18 months old. I had seen him 2 days earlier. Martin had a mild fever. But otherwise he was happy and well. I had advised paracetamol. Joy is now very distressed. Martin has now had a high fever for 24 hours. Paracetamol has brought no Joy to Joy. Nor to Martin. Martin’s fever is still high. There are no other symptoms. No cough. No rash. No runny nose. No sneezing. No vomiting. No diarrhoea. I check him over. He is hot. His temperature is 38.5. He is alert and looking around. But he’s unsettled. Miserable. Not irritable. Martin’s examination is otherwise normal. I have excluded a number of conditions. He has neither malaria nor a UTI. No sepsis. I note that he is fully vaccinated – and had his measles jab 3 days earlier. This seems important.
Then I spot the cannula in his arm. Joy tells me: I came here last night. We have started him on ceftriaxone. Intravenous Domestos. A catch all antibiotic. An understandable approach. Martin’s fever has everyone stumped. On edge and unwilling to miss a treatable rabbit. This rabbit shouldn’t get away. And yet, I know that Martin is not septic. His fever is almost certainly a response to the measles jab. And 16 hours later, Martin’s fever is unabated despite the antibiotics.
Joy remains very worried. Wanting more answers. I think I may take him to Velos. She tells me. Away from the only paediatrician in the District. I don’t say. What will the team there do for Martin? Comes out of my mouth. I could get a full blood count.&nb
Hospital madness - A magician at work
Written by: Keith and Ginny Birrell

Highlight of the week: Close ups with elephants, with no fear
Lowlight of the week: A sick boy with a life sentence
Maximum temperature: 33 Degrees Celsius
Rainfall: Rather dry
The witching hour. Strange medical things that go bump in the night. 02:00 - 04:00. A time best left to the fairies. Not a time for us mere mortals to be troubled. Bizarrely, I have never seen, or been seen, at this time. For the entirety of my career…. So far…. My juniors never needed to call me…..
Evenings in South Luangwa are typically quiet. Gone are our days of raving. Partying ‘til dawn. Going to work on a hangover. Thinking that sleep is for softies. Our middle names are now Responsible. The irrational vigour of youth spent. We crave our due ration of sleep. Downtime part of the mix. Occasional nights out remind us of the heady days of our youth. Yet even those nights fizzle by 21:00. Especially on a school night.
It's 19:30. We have eaten. Taken our antimalarials. Cleared up. Prepared our bags for the morning. It’s wind-down time. I prepare for bed. Crawl under the mosquito net. Read. Chill. The lights should go out at 21:00. But Keith calls out: Don’t get undressed yet. We have work to do.
I’m tired. Bummer. I groan. It has already been a long day. Nowhere near the witching hour. But still, my relaxation plans have been destroyed. Grumpily, I emerge from the bedroom. We steel ourselves for the next bout.
Jack is having some kind of mental health crisis. Can we help? We try to gather more information. We are told that Jack is staying in a camp up the road. He was due to fly out today. But he was too distressed to get on the plane. Could you see Jack? He might need sedation. We do a quick stock check. Oral and intramuscular magic. Cushions for the mind. Medicines that calm and protect. We hop into Mzungu. Our white Hilux. And head toward the camp. Thinking aloud.
Thinking is allowed. Although many clinicians seem to fire from the hip, way too often. A great joy of medicine is the challenge that it offers. No two patients are truly alike. Our shared job as Valley Doc a precious thing. For each conundrum we see things with different eyes. We bring differing views. Approaches. Spin things different ways. Synergistically, not oppositionally. Problems halved or at least shared.
Our journey to see a patient is a crucial phase. Thoughts collected. Approach negotiated. Tasks apportioned. A flexible plan, mapped out. A goal at least. In this way, we arrive with purpose. Our clients see confidence. To inspire confidence. Part of the battle. Anxiety muddies the water. Clarity is needed.
Jack sounds agitated. Clouded thoughts. The product of medical, chemical or psychiatric forces. But we must not jump to false conclusions. Run before we can walk. My task will be to gather information from those around Jack. Keith will aim to engage with Jack.
The phone rings again. There is confusion. Jack is on the move. No longer at camp. His colleagues have taken him to a clinic. But which one? Kakumbi? Or Velos? We stop on the road. Ten minutes triangulating. Velos the new plan. Our drive resumes. Velos is a short schlep. 30 minutes under Mzungu steam.
It’s 21:00. We arrive at Velos hospital in synch’ with Jack. He is sat in the front passenger seat of an open game viewer. Held fast in a caring embrace by a young lady. Settled? We rashly venture. But as we approach, it becomes clear that all is not well.
A flash of anger. Menace. Fearful eyes. Words betray his paranoid state. The car door thrown open. A stare, insistent that Keith should not approach.
Jack’s agitation propels him away from us. Fortunately, the hospital parking lot is a safe space. Well lit. Fenced off and elephant-free. He mutters at nobody in particular. Pacing. His girlfriend heads his way. To shepherd him. At least there is no suggestion of any getaway plan. But Jack’s inner turmoil, and our challenge, won’t be resolved anytime soon.
Whilst our patient mutters and paces, I peel off to focus on my preassigned task. To seek further information from Jack’s colleagues and his partner Lucy. Keith phones a friend. Jack’s best friend. Jack’s brother. Rudi.
No history of fever. No rash. No unusual insect bites. No illness. A four week steady decline in work ability. Change of attitude. Reports of being confrontational. No history of alcohol abuse. No drug use. He hasn’t slept well for the last week. Not at all for the last 24 hours.
Keith speaks to Rudi, one thousand kilometres away. Rudi and Keith share their intel. And then Keith begs a favour: A reference from Rudi that will likely help Keith gain Jack’s trust.
Nothing in the gathered stories suggests an acute medical illness. Nor a toxic response to chemicals. That leaves a psychiatric issue. Acute paranoia. Disturbed thinking, without a physical or so-called organic cause.
The phone is spirited to Jack. Opening an intracontinental dialogue. Initially, Jack’s paranoia puts the kybosh on our preferred way to Jack’s heart and mind. The phone is thrust away. The tarmac impacted by the phone’s resilient case. Strike one. The use of someone else’s phone is eschewed. Not to be trusted. Try harder Doc.
Reaching the end of the opening salvo of our plan: Keith and I reconvene. The plan needs some refinements. Some detail. Some contingencies. Trust is key. A shared plan with patient and docs might involve sleep and calm. Chemically induced calm, for a troubled mind, is best taken by choice. But how do we help Jack to realise that our choice can also be his choice? A photo of Jack’s chosen medicines give Keith an in. Sleepers seem to be an acceptable option. Lucy is tasked to ask Jack if he would like a sleeping tablet. A chill pill. A rest.
Amongst our contingencies is the nuclear option. If anxiety, anger and agitation make it impossible to play the softly-softy approach, our plan B is an injectable chemical cocktail. Designed to go into a big muscle and to work fast. But fast is a relative term. Intramuscular injections take several minutes to down an angry bull. We just can’t fire from a safe distance. We need to be up close and personal. Jab into a held thigh. Hold the anger and the power of the challenged creature. We have a collection of burly security officers and clinicians on hand, ready to hold limbs. To take the strain.
We touch base again with Rudi. Jack’s brother is resigned to a compulsory detainment approach. His words consent to the use of necessary force. Rudi is in the loop. He knows of the need to protect the safety of Jack’s carers. He recognises the therapeutic properties of the proposed sedatives. Keith arms himself. With a mixture of drugs that he is familiar with. Just the right blend of anxiolysis and counter-paranoia. A syringe of the possibilities lies up his sleeve. Yet Keith bides his time. Seeking even now, to find a key to Jack’s heart. A key to Jack’s mind.
The prospect of a scrum, centred on Jack is not relished. It would take away Jack’s dignity and his free will. It’s rarely therapeutic to act in this way. Occasionally a necessary evil. A route toward mutual safety. But it is also a retrograde step. A step backward from trust. After forceable detainment and chemical assault, it’s an uphill battle to re-establish trust. Keith later tells me: that in 24 years as a GP he had never sectioned a patient. Not a single patient, sad, mad or bad, had needed treatment, against their will, in 24 years. I suspect witchcraft. Why else would all of his patients follow the party line, pied piper of Hamlyn style, for all of that time? But I had never seen this wizard casting spells before now.
Jack and Keith dance. Not the traditional steps. But they size each other up. From a distance, at first. Jack brushes Keith off. You are using the wrong words Doc. He chides. Keith takes the verbal punch. But he now knows that he is inside Jack’s armour. Somehow, they end up physically closer. On the floor. Keith ventures an arm. Holds Jack’s back. Physically and figuratively. Keith offers Jack medicines to allow him to rest. To calm his over paranoid mind. They joke about the phone holding Jack no ill will. Keith’s sleeved arm hidden from view. Just because you’re paranoid, doesn’t mean that nobody is out to stab you. Keith laments inwardly.
Keith borrows Jack’s phone to call Rudi. Rudi’s voice calm and measured. Rudi and Keith wrap Jack in emotional cotton wool. They talk of common passions and pet hates. They guide him back to what usually makes him tick. And how to put his tick back.
To read the rest of this blog, click on the link: Hospital madness - A magician at work / BLOG | Into Africa