Sleeping sickness two
Written by: Keith and Ginny Birrell

Highlight of the week: Our last weekend Sunday in the park with Perry - our top friend and guide who last week passed his level 1 guiding exams - and came top in the country. Nothing but the best for us.
Lowlight of the week: It dawns on us that we are leaving here next week. A house to pack up. Bags to pack. Goodbyes to be said.
Maximum temperature: 43 degrees Celsius
Rainfall: Looking forward to saying yes next week as we return to a wet cool October
Let’s swap beds for a night! The space next to Keith can easily accommodate any morphology. We have a king sized bed. We use a light sheet and keep the aircon on. All night. And the fan to boot. And yet somehow sleeping in the oppressive Zambian summer is problematic. A sleeping sickness, of a sort, is afflicting me. And so you are welcome to swap beds with me. For a trial run only.
I tick a few boxes for the possibility of all sort of maladies and hormonal misfires. At the age of 59, I’m well past my natural menopause and my hormones come nicely packaged up in a box. Strike one. My night sweats are not peri-menopausal. Perhaps we should consider TB? Keith has been coughing for an age. He reckons he’s allergic to Zambia. The sneezes are quite a thing. Not quite typical of TB. Strike two. The fatigue that accompanies sleep deprivation, combined with doubly sapping daytime conditions, even has me mooting cancer. But that is easily scrubbed out. Strike three.
The honest truth. On reflection. Is that 24/7 responsibility, in itself, almost has us on our knees. Tired. Burnt out. Call it what you will. A 3 month stint here is quite enough. How did we ever do 6 months in 2021? We really deserved a medal, Muttley-style. For services, above and beyond the call of duty. We left with nothing, but scabies.
I crave a day off. Proper down time. The opportunity to light a fire, on an autumn evening, in Yorkshire. To snuggle under a 13 tog duvet and to need it. To listen to the night sounds, without the constant hum and drone of dual aircon and fan. Even chortling hippos, roaring lions and barking baboons stay masked here. I crave the hoot of my Yorkshire owls and the peace of still cold nights.
Sleeping sickness is affecting our Valley in more ways than one. Tryp is a fussy little fellow. Rare and very niche. But other sleeping ailments also exist. My drenching night sweats might not be particularly pathological, but they mess with my crystals and chakras nonetheless. Perhaps I should move on? This blog is not meant to be all about me.
Let’s talk about William. He is this week’s case study. His need for attention is greater than mine. He is currently out of work and unemployable. All because he has a sleeping sickness. Not tryp you understand. His story doesn’t fit with tryp. William would have you believe that his problem started about a year ago. The rot started well before that. But more of that later. The bottom line is that tryp can’t be the cause of William’s woes. If it had been, William would have been dead and buried at the end of last year.
William is a 42 year old guide. By all accounts, he is the bees knees. Skilled. Knowledgeable. Amenable. A favourite with his guests. But only when he is awake. And here is the crux. William has a tendency to fall asleep. At the drop of a hat. And that hat seems to drop all the time. While sitting down chatting. While at the bar getting a drink. But more importantly, while at the wheel of his safari Landcruiser. A big issue when he is driving guests in the park. Picture this if you will. Narrow dusty tracks. Steep drop-offs, next to a crocodile infested river. Trees. Elephants. Hippos. Too many obstacles for his now autonomous vehicle to navigate driverless. Guests have had to grab his steering wheel. Give William a sharp nudge in the ribs. Relaxing game drives in the park have become white knuckle. Not surprisingly, William has been sacked. Again.
We find William serendipitously. A chance encounter with William’s boss. Keith’s ears prick up at the story. As part of our stroke prevention programme, we screen for obstructive sleep apnoea. A condition linked to hypertension, type 2 diabetes and strokes. Mainly caused by obesity. As a person drifts off to sleep, the muscles in their neck relax. The fatty tissue in the neck becomes unsupported. It compresses the upper airway. Typically, a person snores loudly. And then has a pause in their breathing. Which lasts for 10 to 30 seconds. Followed by a gasping intake of breath. The person has been suffocated by their own body. This happens repeatedly overnight. Leading to a poor night’s sleep. And then daytime sleepiness. A tendency to fall asleep easily. In meetings. Whilst being driven. And occasionally whilst driving. A plan is hatched. Keith will see William. Diagnose his problem. Enrol him in our stroke prevention programme. And help William to help himself.
It's Monday morning. Par for the course, there is already a line of patients to see Keith, as we arrive in clinic. WhatsApp sounds off. Morning Doctor Keith. William here. I am waiting for you. I am wearing a red checked shirt. We scan the waiting crowd. And do a double take. There is just one person in a red checked shirt. A smart, smiling man. But he is the wrong shape for us. He has defied our expectations. Tall and slim. His waistline is just plain wrong. Sleep apnoea seems only an outside bet now.
Keith works his way through his morning queue. William is patient number three. A quiet space is found. William is able to tell his story. He describes some sleepiness. A poor sleep pattern at night. He recollects it starting just about a year ago. After a short illness. Keith asks some directed questions and works out his Epworth Score. Epworth Hospital is a sleepy place in Australia that has 2,000 beds. Their scoring system just tells Keith that William tends to fall asleep a lot during the day. William scores 18 out of a possible 24. But William is keeping schtum about what happens when he drives a car. A common white lie. As Keith documents the tale, William drops off and has 40 winks. And Pinocchio’s nose gets a little longer.
William’s slightly sugar coated tale of woe also involves a poor sleep pattern. Night time comes and he barely sleeps at all. Two hours on. 2 hours off. Perhaps repeat. Never refreshed. Schrödinger’s cat is either asleep, or not asleep, in this particular box. But the cat needs a firm diagnosis to fix this sleep disorder conundrum. For now, Keith parks the conundrum with some melatonin and some sleep hygiene advice.
Keith is a bit of a whizz with sleep apnoea. He has a tool kit of remedies for that all too common affliction. But his gut instinct is that William has something altogether different going on. He decides to phone a friend.
Meanwhile, we happen upon William’s ex-boss. We tell him that at least William is playing ball. Engaging in the medical process. But his boss is still worried. The story from William does not add up. This problem has been recurring for years. William has lost a good few jobs from falling asleep at the wheel. He has gone to other parts of the country to work. But his sleepiness has travelled with him. This bad penny keeps cropping up. Perennially out of work.
Everyone needs friends. And many of you know that we aren’t always the best of correspondents whilst we are in Zambia. Except, that is, when we really need you as a friend. And so our friendship is rekindled. Shamelessly. Our first friend Simon recommends that Paul might be a better friend to us than he. Paul happily, is a sleep specialist. A friend indeed. We set up to rejuvenate our friendship.
We hate to admit that Mr Musk has any virtues whatsoever. But his starry connections guarantee a decent chat online. For social intercourse and even for work. Paul is a mine of useful information. William likely has narcolepsy. In effect William gets a tertiary specialist opinion, In Africa. Within a week.
Paul shares that the proof of the pudding is in the eating, as far as narcolepsy is concerned. There are some tells. Vivid dreams, especially during the day. Poor night-time sleep. Positive emotions triggering sleep or blank episodes. But Paul advises that tests are rarely important. My ears prick up at this. This is right up our street. Well down our sandy track at the very least. We specialise in not doing tests. What have you got to lose by trying him on the right medicine for this? says Paul
Baclofen, an underused drug, is available here, at a pinch. It helps people with narcolepsy get some restorative sleep. And modafinil. Basically an on switch, to combat William’s perpetual tendency to be switched off. William will need to be paced, to get the balance right between the ons and the offs. After being on for 4 hours during the day, he will need to nap for 30 minutes. Off. That could be just right for a guide who’s drives last for about 4 hours.
The ink is barely dry on the first page of William’s notes. As a guide, he gets to be part of a private medical programme, that should pay for his drugs. There is light at the end of the tunnel for him. A bright light during the day, to keep him awake, and a soothing dull night light to cushion him, as he takes restorative sleep. Medications and good sleep hygiene. Hope for William. To allow him to take the wheel again. To allow him to share his passion for nature with his guests. His Landcruiser currently off limits.
William and I are in a not so exclusive club. Sleep disorders are a motley collection of some common or garden varieties and some rare and fascinating maladies. But more people have occasional sleep issues than not. And more than one in ten of us is chronically afflicted. Sleep apnoea for example, affects 10% of our camp staff. William’s problem on the other hand is almost esoteric. He is special. Perhaps only 1 in 5,000 people are affected. But it’s not esoteric to William. William needs to know. He needs to know about his sleeping sickness. And so do Paul and Keith.
Tryp... tryp... tryp. A pain in the bum
Written by: Keith and Ginny Birrell

Highlight of the week: We dance our way out of clinic. There is no cure for our strange gyrations. We are compelled to dance for our lunch. But at least it’s a free lunch for our staff.
Lowlight of the week: The party is over. This is our last full week as Valley docs.
Maximum temperature: 42 degrees Celsius
Rainfall: The forecast suggests that our seasonal rains will be lower than average. Average at best.
t’s 1905. South Luangwa is in splendid isolation. Dual forces are at play. Forces hell bent on depopulating our Valley. A deadly illness is affecting colonial settlers. Sleeping sickness. Colonial authorities declare South Luangwa a no-go area. Cattle and men go home. The wildlife go wild. This is the beginning of South Luangwa as a conservation hotspot.
It’s Sunday. One hundred and twenty years later. Our day of rest. We charge double rates on a Sunday. To deter the not-so-sick from calling us. We plan our day: a drive in the park; a bush breakfast and coffee; home for a late brunch; a relaxing afternoon; a dip in the pool to cool down; a comforting evening meal; early to bed.
But our Sundays rarely go to plan. It’s Zambia, don’t you know? We start with a kerfuffle. None of our guide friends are free. Their open game viewing vehicle is double-booked. Plan B is a self-drive. It’s Joel’s last day here. We can’t not go in the park today. Breakfast is made the night before. Bags readied. Kettle full. Coffee grounds await.
05:00. The dreaded alarm clock goes off. Still dark. Silent. The baboons are very sensibly still sleeping. We drag ourselves up. Shower. Dress. Boil the kettle and make coffee. Fill the cool bag with breakfast and cold water. In the car by 05:45. At the park gate by 06:00. We glean some info from a guide. There may still be a leopard up a tree. With a kill. On the way to Wafwa. I saw it last night. It’s 50:50 that the leopard is still there.
The uncertain post prandial habits of a leopard determine the direction of our drive. We turn right down Mushroom loop. En route to Wafwa. The Dead Luangwa. A now dry oxbow lake. But our instructions are vague. The candidate trees numerous. I swear I look up all of them. No leopard to be seen. But that’s fine. The park is peaceful. We watch a herd of elephants lazily walk to the river’s edge. Drink. And turn around. Three giraffe go one step further. Into the water. They cross the river, right in front us. The water barely laps their ankles. Scarcely. Drought the word on our dry lips.
We continue to head north. Chipela Chandombo Lagoon our breakfast oasis. One of the few lagoons in the valley still holding water this year. Mzungu’s doors open cautiously. A lone hippo plays dead in the lagoon. No threat here. We alight and drink in the scenery. We drown our breakfast muesli with milk. Coffee also rehydrates us.
It’s 08:30. Breakfast is serene. Birds flying. Impala drinking. Peaceful. Quiet. We listen for alarm calls as ever. Expecting the bush telegraph to warn of danger. But there are none. Our breakfast time sacrosanct. We savour our breakfast. On cue the serenity is broken. By an unwelcome harbinger of doom. An annoying little ringtone. An insistent chirrup. An alarm call of sorts. The Doc phone. Hi guys. Sorry to bother you. My husband has a bite. I think it might be a spider bite. But I am worried it could be a tsetse bite gone bad. All this talk of sleeping sickness has us worried sick. Can you come and see him?
A picture arrives through the ether. A lesion of interest. A possible chancre. A purple ulcer surrounded by redness. All that is missing here is the story of a painful tsetse fly bite in the preceding days. Our interest is piqued. Mzungu becomes FAB1. I become Lady Penelope. Parker, my loyal chauffeur, engages the Rolls Royce thrusters. We head off to clinic. Thunderbirds are Go!
Let’s take a short intermission here to tell you a bit about Trypanosomiasis. Easy for you to say. Most medics here call it tryp. To avoid tripping over their tongues, most likely. Sleeping sickness is the lay spin on it. Tryp is a parasite spread by tsetse flies. Bastard flies sums it up. With chainsaw mouthparts. They bite through clothes. Boy flies and girl flies both bite. At least they aren’t sexist. Neither gender gives a figs arse about DEET. Not caring that they hurt when they bite. Oh and tsetses are almost immortal. Armour plated. A full Newton force is needed to crush their robust bodies. An apple dropping from a decent height onto hard ground might just do it.
There are 2 forms of tryp. In West Africa tryp causes a chronic, protracted illness. Trypanosomiasis Gambiense takes weeks to months to wear you down. Leading to a gradual decline in health. Your brain function muddies up. Altered sleeping patterns. Eventually it is fatal, if not diagnosed and treated. But Trypanosomiasis Rhodesiense is much more aggressive. Found in Eastern and Southern Africa. A fast burn. Symptoms appear 7 to 10 days after a painful bite. Then comes an ulcer surrounded by anger. The chancre is often not especially painful. But it usually looks angry. Fever. Headache. Muscle and joint pain follow in short order. The parasite makes a beeline for the brain. Wreaking havoc on brain functions. Confusion. Delirium. And death is inevitable without treatment. Within 4 weeks or so.
When we first came to the valley in 2021, tryps seemed to be asleep. Our predecessors knew nothing about its latent ways. The received wisdom being that sleeping sickness has been properly put to bed. I won’t be needing to know about that. I delude myself. The tryp parasite disorganising my thoughts already.
Two years tick by. It’s 2023. I am doing my DTM&H course. Tropical medicine. And let’s not forget that critical hygiene part. Diseases around the world are now my daily diet. I want to cope with the bugs and nasties found in South Luangwa. But I’m forced to take in the also rans. Fascinating and alien-like parasites, but surely they’re all irrelevant to me? My remote course in Glasgow goes big on Tryp. A whole week of my timetable seems focussed on this niche ailment. I plan to doze through the lectures on tryp. This could be a big turn off.
The timetabled tryp week kicks off. I have a pillow at the ready. Next to my computer. But as I practice closing my eyes, Professor Lucille Blumberg appears on my screen. From Johannesburg. South Africa. Lucille opens my eyes. Wide. She presents a series of cases. Tourists on holiday. Many from South Luangwa. At this point I cancel the day dreaming plan. I’m in the room. Well, the virtual room, at least. Six cases since 2011. Not common. But ever present. After the lecture, I stay online. For a private word. I explain that we have been told there is no tryp in our Valley. This seems to be a mistake. Closing our eyes to the sleeping beast. Potentially this approach is responsible for late presentations and avoidable deaths. I now have a hot line to the Human African Trypanosomiasis expert.
This year the sleeping beast has awoken in our valley. The first confirmed case of tryp in 6 years was in April. Three months before we arrived. The diagnosis was delayed. The incumbent doctors were late to the party. Confounding factors confounded them. A plan is made, to play things better next time. Experts in South Africa arrange meetings. Zoom clicks into action.
It’s June. We are at Manchester airport. Being Trumped by the Qatar air traffic control shutdown. Fireworks cross the Gulf skies and we are stranded. I stand in a queue for 2 hours at the Qatar desk. Keith is on a conference call with Lucille and Evan Shoul amongst others. About Tryp. They discuss education campaigns. Raising awareness. How do we ‘fess up that there is still tryp in the valley after all? Might the tourists stop coming? A plan is made. Tourists and locals should watch out for painful bites going bad. Increased surveillance. Information sharing. And a plan of action for suspected cases. Photos of lesions of interest. Communication.
There is a new kid on the block. The tropical health block that harbours our specialist colleagues Lucille Blumberg and Evan Shoul. A wonderkid. A new, safe, drug that kills tryp, dead. Treatment these days for tryp should be straightforward. But there is a but. Delay in diagnosis, or delay in starting treatment, and our noxious, antisocial, parasite has a field day. Munching up brain tissue. Irreversibly scrambling neurones and their vital connections. The wonderkid is taken as a course of tablets. A little monitoring is needed. But otherwise the little Pac-Man style brain munchers are sent packing in short order.
But until this week the wonderkid drug is a little hard to come by. Fexinidazole. Held centrally by WHO. Apparently there is no Fexinidazole held in Zambia. That’s all well and good if you have medical insurance and can get to Jo’burg. Where Lucille and Evan will guard your back. And most importantly they will guard your brain. But it’s not so good for lowly Zambian farmers and safari staff. Who might just languish on understaffed wards, waiting for an elusive test. Dying in want of a diagnosis. Invisible to WHO surveillance. No disease. No drugs. Chicken. Egg.
Testing is also an issue. There are no quick and easy tests for tryp. Skilled laboratory technicians are required. Most lab staff have been taught from the same faulty song sheet. With the wrong music. They tell us that blood needs to be taken between 01:00 and 04:00. Plain wrong. Any time of day will do. No one wants to be up during the witching hour. So many don’t test. And that usual test is pretty tricky to do well. The sleeping tryps stay cloaked, masquerading as common or garden malaria or meningitis. No known sleeping sickness. No notification to WHO. No need for drugs to cure it. Get the supply chain wrong. And no supply. Unknown unknowns our problem here.
Let’s return to Sunday morning. We beat a hasty retreat from the park. Our patient, Bruce, meets us at clinic at 09:30. He looks chipper enough. Walking wounded. A pain in his bum. At the site of the bite. No fever. A mild headache. General aches and pains. We examine the bite in more detail. And share the uncertainty. WhatsApp style. Our WhatsApp group is super high powered. Lucille, Evan, ourselves and Franklin. Franklin the top tryp doc in Zambia. And then we place our bets. Each of us ventures our opinion.
Certainly it’s not typical of a tsetse bite gone bad. Still a tryp chancre is at the top of our list. It needs to be ruled out. The story, and the lesion of interest, both point to a spider bite, or a tick eschar. Spider toxin leaves doctors all at sea. We have no tools in our kit for that. But at least tick bite fever is easy to treat. We’ve talked a lot about our favourite test before. Time. But tryp steals time. We can’t wait for time to make our diagnosis. We can’t wait for the deadly Pac-Men to munch on Bruce’s brain to give the game away. Time waits for no man. Our problem is time critical.
It's Sunday. There is a skeleton staff in the clinic. No duty lab technician. Lucille’s words echo in my head: Get a drop of blood. There’s no need to stain it. Look down a microscope at a low magnification. Fresh tryps will dance. But my enthusiasm is instantly dashed. The first hurdle too high. The lab is locked and the key is out of town. Drat. And double drat.
But Keith holds the ace card. He plays it with a flourish. Gloria promised me that she can test for tryp should the need arise. He announces with a smile. He barely supresses a smirk. I’ll message her to see if she is available. I stay quiet. Not wanting to dash Bruce’s hopes. Sunday remains the Sabbath in Zambia. The best we can realistically hope for, is a test on Monday.
I close my eyes to let the sleeping sickness take me for a moment. But when I open them Gloria fills my view. In her Sunday best. Straight from church. Lady Penelope stands down. Gloria who works for the fisheries and wildlife department, has access to the holy grail. A laboratory with microscopes and a PCR kit. To cut a long story short: she even has the ability to detect the minutest particles of tryp DNA in blood. It will take a few hours. It needs laboratory graft. But if we provide the blood, Gloria can do the tests. Our patient rolls up his sleeve. Blood is drained from a vein. And off Gloria goes. Promising to contact us in 4 hours. With the result.
Nobody has placed a bet on Tryp. Yet it’s still on the table. Our WhatsApp group plans for contingencies. We chase the elusive Fexinidazole. The word on the street is that, despite assurances that it can be made available within 24 hours, it would take 5 days to arrive in Lusaka. Five days that Bruce does not have. We treat Bruce for the treatable. That includes doxycycline, a simple antibiotic that does for tick bite fever. Best taken on a full stomach and not just before you sleep. We warn Bruce not to sleep after taking his antibiotics. And we say a silent prayer, on the Sabbath, to ward away sleeping sickness.
Its 17:00. We are driving to the airport. Joel is off on his adventures. After a month cooped up in Kapani and Kakumbi. Joel leaves our nest a little empty. He fledges and aims to flit around. Two months of fluttering around Botswana. Namibia. Possibly South Africa. The phone starts to warble again. It’s Gloria. The PCR is positive. Bruce has tryp.
Organising Bruce’s ongoing care involves a familiar and frustrating battle. Another insurance company trying to save dollars. I can’t bear to describe the convoluted dance that Bruce’s wife, myself and the monkeys representing Bruce’s insurance company have over the next few hours. We have grumbled about this process before. A battle I always seem to win. But the protracted campaign tests my grit and Bruce’s wife’s resolve. Bruce’s unscheduled trip with tryp to Jo’burg is magicked as a consequence of my 13 years training to be a doctor and my 18 years in practice. This Valley has invested in Valley docs for one main reason. We can do magic.
Drip, drip drip
Written by: Keith and Ginny Birrell

Highlight of the week: We jointly retain the Silver stool award for 13 weeks1
Lowlight of the week: Joel leaves us for fresh adventures, starting in Livingstone.
Maximum temperature: 45 degrees Celsius
Rainfall: Some in Tafika – 2 hours north of us
Drip, drip, drip. The Chinese water torture of our ailing air conditioner in the wee small hours. Keith jumps up. He saves our bedroom furniture with prompt action. The air conditioner goes off. The fan goes on. At turbo power. The drip stutters and stops. The fan blows the skitters hard against the outside of our bed net. Mrs Mosquito’s night time campaign fails. Fans at night become the new normal.
Gastroenteritis. Diarrhoea and vomiting. A gruelling ailment that sustains our practice, yet drains us personally. Best avoided. Fluid issues from both orifices without invitation. Drip, drip, drip. Fluid issues are the main way of managing our unfortunate patients. A worldwide affliction that challenges high income countries too. But in low and middle income countries, poor access to water and excess heat often add insult to injury. Zambia has more than its fair share of D&V. Children can get super ill, super quickly. Early pick up and early hydration keep the Grim Reaper at bay. Dehydration a killer. On a background of marginal nutrition and chronic worm infestation. We have to be on our toes.
My ward round at Velos this week is a slow burn. I arrive on the ward at 09:30. Helen, the nurse in charge, is delighted to see me. She readies the trolley for the ward round. Looking at me expectantly. But that is not the deal I have made. I am not here to do ward rounds by myself. I am here to support. Teach. Encourage good practice. I decline to start the round. Let’s wait for the team I suggest. Whilst waiting: I take the opportunity to review the notes. We have 5 children to see. The first is in bed one. Beds 1 and 2 are nearest the nursing station. These beds have piped oxygen. The sick kids get put here. I see a bundle of blankets on bed one. A little mite, Martha, wrapped up in them. Mum is expressing breast milk into a small container. I read the notes. A 5 month old baby. Weighing 4.5 kg. Drastically underweight. She presents with diarrhoea and vomiting. Assessed to have severe dehydration. Her malaria test negative. An IV cannula is inserted. She is given some IV fluids overnight. But the IV is no longer running. She has no fever. Her heart rate is a little fast. Everything else is pretty normal.
Martha’s mum has expressed a full bottle of milk. But it sits idly on the bedside cabinet. For 45 minutes. Until our round kicks off. No fluid passes Martha’s lips. No drip, drip, drip. No life fluid imbibed. No fuel to the carburettor. But at 10:15 the throttle is engaged. My slow start finally speeds up. Misheck, the clinical officer, arrives. Martha is our first patient. Bed 1 seems a good place to start. Martha’s thirst needs quenching.
Martha’s story is reviewed with mum. We are relieved to learn that the baby has not vomited since 02:00. But she has had 4 loose watery stools since then. She looks sleepy. With a dry mouth. The soft spot on top of her head is sunken. Her fontanelle is a window into the water pressure inside her head. Her skin is loose. Very dehydrated.
Mum tells us that Martha is too sleepy to go on the breast. She does not have the energy to suck. What’s your plan team? I enquire. Misheck says that they will put up more IV fluids. Shall we just try some oral rehydration solution (ORS), pang’onopang’ono? The Nyanja word is a challenge for me to say. But it helps to say it slowly. With an open mouth. Slowly, slowly. My plan is met with withering looks. She is too sick to feed. She has no energy. But Martha’s open mouth mirrors mine. Surely she will want to quench that thirst.
I reach into my bag and find a 5 ml syringe. I fill the syringe with ORS. I put it into her mouth. Martha’s first reaction is to turn away. But then she takes more interest. I slowly push the ORS into her mouth. She gives a weak cry and starts to swallow. The syringe empties quickly. I refill it and repeat the process. She swallows more keenly. But I stop. Do this too fast and Martha will vomit. I give our nurses instructions to give her one syringe every 5 minutes. That’s one millilitre per minute. 60 millilitres in an hour. We share the plan with mum and get her involved. And then move on to bed three. We tell mum that we will see her again shortly.
Playing Sh**head2 with beds, we miss out bed two. It’s empty. Waiting for another touch and go child. A child who would have to be perilously ill. Bed 2 is strategically vacant. Bed three usually holds, by definition, a less sick child. But bed 3 is also empty. Nathan is 2 years old and is up and running around. He came in with severe malaria, 2 days ago. Two days of treatment sees Nathan off the critical list and ready for discharge.
At this point I glance back at bed one. I have been watching Mum struggling to take the lid off a sugary yoghurt drink. I assume, in error, that she is going to give herself an energy boost. Unhealthy for her in the long run, but at least this drink could keep the wolves from her door today. Once the lid is off, to my horror, she starts giving the yoghurt drink to baby Martha.
Our game of S**thead jumps back the way. Back to bed one. I insist that mum needs to be taken to task. We find the smoking gun. And the fastest gut in the South is explained. Martha’s gastroenteritis links to poor feeding practices at home. Babies should be exclusively breast fed in Zambia until 6 months of age. It is impossible to sterilise bottles here. All the nutrition they need is present in breast milk. From a clean package. Kept safely at body temperature.
Mum admits that she has been giving baby Martha yoghurt and porridge. The confession clears the air. The maxim that mother knows best only applies when education is a birth right. And that is not yet true here. Somehow Martha’s mum thinks that yoghurt and porridge are better than her own milk. The milk that she has so patiently expressed and kept to one side. She gets a good talking to. Sorry let me reframe that: She has a guided conversation to better understand the impact of her health decisions. Education. Encouragement. Support.
We finish the round by 11:15. I return to bed one. Mum has given all the expressed breast milk to Martha and is now expressing some more. She has also given the baby 8 syringes of ORS. Martha is alert and looking around. Two hours ago she was deep in a perilous jungle full of invisible pathogens. Now she is still amongst the trees. But she is at least on the right track. The track that leads back to the safe plains. Away from the bugs and unsafe waters. Unsafe water is replaced with safe water. Breast milk and ORS to be precise.
Fast forward to Wednesday. Our clinic day in Kakumbi. The day starts slowly. The computer system is on and off. Still unreliable. I am called out to the reception area. There is a 18 month old child for me to see. Mwiko is in his mother’s arms. Looking listless and disinterested. A bit floppy. We usher them into the consulting room. Keith sits to write some notes. I do the doctoring. Mwiko has had diarrhoea and vomiting for 3 days. He is still vomiting everything they offer. The last vomit was an hour ago. He has loose watery stools. Another case of gastroenteritis. We have seen a few cases today. All purging their intestines to a varying degree. All feeling a bit sorry for themselves. Not properly wrung out. But Mwiko takes the biscuit. Or rather, he is the poster child for bathroom visits. Mwiko is different. Dry mouth. Reduced skin turgor. Lethargic. Dry McDry from the clan McDry. He is moderately to severely dehydrated.
I ask Keith to fetch a magic bullet. An anti-sickness tablet. Ondansetron. Its local trade name is Vomikind. In my humble opinion Vomikind is the best named drug ever. It works so well. Dissolving in the mouth. It is absorbed super quickly. And it rapidly knocks off the vomit switch in your brain. Kindly. We pop a tablet in Mwiko’s mouth and take him around to the ward. I give instruction to give ORS slowly. A plastic bottle is quickly procured. One litre of ORS is made up. I tip some into a cup and produce a 10 ml syringe. Mwiko is keen to take it. He gulps down the first 10 mls. We have to be careful. Dehydration causes thirst. If he gulps a load of ORS down too fast, it will come back up. Fast. I give instructions. One syringe every 5 minutes. No more. Drip, drip, drip.
One hour later, we go to review Mwiko’s progress. He is sat up in the bed. Smiling. His mouth a bit wetter. I take the syringe and refill it. Mwiko happily takes the business end of the syringe in his mouth. He drinks another 10 mls. We are onto a winner. He is ready for discharge home 2 hours later.
A simple solution. ORS. There is a tendency to rely on intravenous fluids in Africa and Europe. Especially when a child is vomiting. There is certainly a place for IVs. Particularly when a child is shocked and at death’s door. But I have been able to transplant a bit of my own UK practice here. Demonstrating that simple measures are usually enough. Be kind to the vomit centre. Go slowly. A perfect fit for Zambia. Drip. Drip. Drip.
Editor’s note (Keith): Ginny’s humble opinion about her ability to pass on simple solutions to widespread problems doesn’t quite cut the mustard here. I make no apology for editing Ginny’s words and for bigging her up. She is too bashful to do this for herself. The girl is a legend. This simple approach has transformed the quality of care provided in both of our main places of work. Kakumbi and Velos now know how to care for our most common affliction. Doubtless this knowledge will save many more lives. Ginny hasn’t just taught our staff to fish. She has given them a lifetime supply of fishing tackle and bait.
1. The Solid silver stool award. A weekly award given to the owner of the firmest stool on Unguja Island (Zanzibar). Only VSOs between 1994 and 1996 were eligible.
2. Sh**head: a card game in which the objective is to get rid of all of your cards, before your fellow players can outwit you and refill your hand with cards, evoking a fairly negative response.
Intelligent Practice Solutions
Written by: Freya Keith

Introducing IPS: Intelligent Practice Solutions
Richard; business manager of a thriving GP practice in Durham and customer of Dene Healthcare has kindly shared the below information about his new venture, Intelligent Practice Solutions (IPS). As part of Dene’s commitment to letting our customers know about services that can help you and your practice, we are extremely happy to share IPS with you!
At IPS, we deliver intelligent, hands-on business and operational support for General Practices and Primary Care providers. With over 10 years’ experience in General Practice, and still actively working within Practices, we understand the pressures you face and the solutions that genuinely work.
Our focus is on simplifying the complex from managing expenditure and identifying cost savings, to building powerful Excel-based reporting tools that provide business insight at the click of a button.
We’ve helped Practices take control of their finances with solutions for superannuation reconciliation, payroll summaries, and cashflow forecasting. And we don’t just advise we implement change, embed systems, and ensure they deliver long-term value.
Whether you're a Practice Manager, GP Partner, or PCN lead, our support is practical, experienced, and built around the day-to-day realities of Primary Care.
IPS - No problems. Only solutions.
"My experience of working with Intelligent Practice Solutions on several projects has been professional yet inspiring. If you’re looking for innovation, fresh thinking, and enthusiastic support, I would highly recommend. Individually Richard and Jemma each have a wealth of knowledge and experience, both within Primary Care and in the private sector. Working together, their skills sets compliment each other perfectly, allowing them to suggest and create workable solutions to complex issues with a modern ‘thinking outside the box’ approach." - Louise Thomas NHS
"IPS brings a clear and structured approach that enhances accuracy and saves valuable time. Their ability to bridge the gap between day-to-day financial operations and the specific reporting needs of NHS practices has genuinely added value, both to our work and to our clients."- George Swinbank BA ACA - Sanders Swinbank
"We found Richards Xero training invaluable. Removing the use of Dext Prepare has made reporting easier and far more accurate. General Practice requires a far more tailored approach, and this is exactly what Richard provides. I can't recommend IPS enough." - Judith McKeown Finance & Contracts Manager
Click here to visit the IPS website
Healthtech-1: Free your team from manual registrations
Written by: Freya Keith
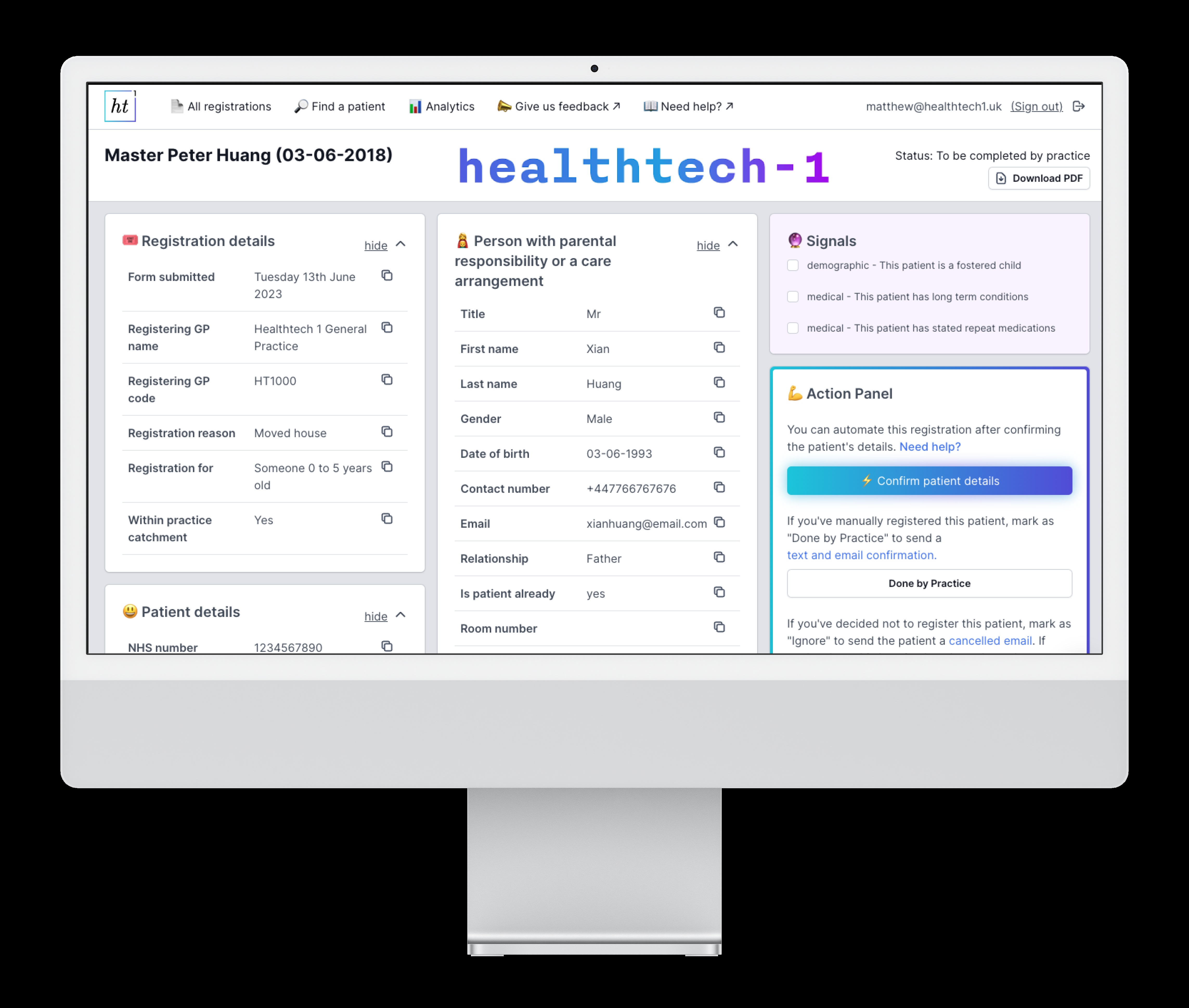
Healthtech-1: Free your team from manual registrations
At Dene, we only recommend services we truly believe in. Healthtech-1 caught my attention for one simple reason — it would have made life so much easier back when I worked in a GP practice.
Created by the son of a GP, and still based in Stratford Village Surgery in East London, the software was developed with a unique understanding of how Primary Care works!
By producing software to automate GP2GP administrative function and patient registrations, Healthtech-1 have already saved over 200 years of NHS time and counting to the 1400 practices using them today!
What Healthtech-1 Does
Born inside a real GP surgery during the COVID-19 pandemic, Healthtech-1 was built by people who know exactly how registrations weigh down practice teams.
Today, Healthtech-1 is:
- Automating up to 99% of new patient registrations
- Trusted by more than 1,450 practices nationwide
- Capturing richer patient data through a configurable local form (beyond the core NHS form)
- Coding everything directly into EMIS or SystmOne
- Recognised as an NHSE-selected provider of automation
The result? Hundreds of staff hours saved, fewer errors, and faster access to care for patients.
Why It Matters
Every practice manager knows the workload that comes with registrations — forms to check, data to key in, mistakes to chase. It’s repetitive, time-consuming, and it pulls staff away from patient care.
Healthtech-1 takes registrations off the to-do list. That means:
- Shorter registration times and quicker access to care for patients
- Less admin pressure on already stretched teams
- No more double-keying or backlogs
- QOF points captured automatically
What Real NHS Staff Say
“I’ve been registering patients for 20+ years — you have no idea how much stress this saves. It meant I could go on holiday during university season for the first time!”
— Sue, Registration Clerk at Claypath & University Medical Practice
“I haven't been so excited since the day the Spice Girls said they'll get back together!”
— Denzil, Registration Clerk at Hurley Group Practice
“I liked the confidence Healthtech-1 had by making their contract breakable at any time. After using it, you wouldn't dream of cancelling! A fabulous invention.”
— Philip Heiden, St Paul’s Surgery and Adelaide Medical Centre
Ready to Find Out More?
If you’d like to see what Healthtech-1 could do for your practice, get in touch:
Contact the Dene team at info@denehc.co.uk to arrange a chat with the Healthtech-1 team. Or use this link to book a call: https://link.ht1.uk/DeneHC